Published On Sep 5, 2023
Cardiac cycle events can be divided into systole and diastole. Systole represents contraction, while diastole refers to relaxation.
The cardiac cycle can be subdivided into seven phases – atrial contraction, 3 phases of ventricular systole (isovolumetric contraction, rapid ejection, and reduced ejection), and 3 phases of ventricular diastole (isovolumetric relaxation, rapid ventricular filling, and reduced ventricular filling).
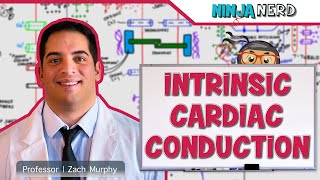
Atrial contraction starts with an electric impulse in the SA node. The electrical signal depolarizes the atria, which contract and pump blood into the ventricles. There is a delay once the signal reaches the AV node. It ensures the atria have fully contracted, ejected their blood into the ventricles first before the ventricles contract.
Isovolumetric contraction. The volume of blood in the ventricles remains constant while pressure increases. As atrial systole ends, the ventricles begin to contract. Because both the AV and semilunar valves are closed, blood volume in the ventricles stays constant, while ventricular pressure rises rapidly. Because ventricular pressure exceeds atrial pressure, AV valves close, preventing the backflow of blood into the atria.
Once ventricular pressure exceeds pressure in the aorta and pulmonary artery, we enter rapid ventricular ejection. The semilunar valves open, there is a sudden ejection of a large volume of blood from the ventricles into the aorta and pulmonary artery. Atria begin to accumulate blood from systemic circulation and the lungs.
Reduced ventricular ejection: blood continues to leave the ventricles, but not because of ventricular contraction - due to the blood’s inertia.
Once the pressure in the ventricles falls sufficiently, the semilunar valves close.
Now, all four valves are closed. No blood enters or leaves the ventricles – hence isovolumetric ventricular relaxation. Blood volume in the ventricles stays the same until ventricular pressure is less than atrial pressure.
Rapid ventricular filling: atrial pressure exceeding ventricular pressure makes the atrioventricular valves open, allowing blood from the atria to rush into the ventricles.
Reduced ventricular filling: during phase 6 and 7, the ventricles receive 90% of the blood they will pump out. The remaining 10% is acquired during phase 1 of the next cardiac cycle.
Pressure changes over the course of the cardiac cycle in the left atrium, the left ventricle, and the aorta: During atrial contraction, there’s an increase in pressure in the atria. There is a slight increase in ventricular pressure as the atria pump blood into the ventricles and ventricular volume increases. During isovolumetric contraction, there is a rapid increase in pressure in the ventricles as they contract and the AV valves close. But the pressure in the left ventricle does not exceed the pressure in the aorta so the aortic valve remains closed. When pressure within the ventricles exceeds the pressure in the aorta and the pulmonary arteries, the semilunar valves open and we enter the rapid ventricular ejection phase. As the left ventricle ejects the blood it contains, the pressure in the left ventricle and the aorta reach their peak. During reduced ventricular relaxation, ventricular pressure starts to decrease, and the blood keeps being ejected due to the blood’s inertia. During isovolumetric relaxation, pressure decreases in the ventricles, as they relax. Aortic pressure exceeds left ventricle pressure and the semilunar valves close. Blood starts to flow back to the heart, which causes a dip in aortic pressure. Blood volume in the ventricles remains the same until pressure in the ventricles is less than that in the atria. Once atrial pressure exceeds ventricular pressure, the AV valves open and we get rapid ventricular filling. This results in a swift decrease in atrial pressure. During reduced ventricular filling, aortic pressure continues to fall.
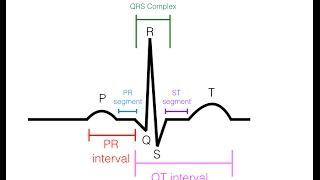
An ECG is a visual representation of the cardiac cycle’s electrical events.
The P wave is a small upward deflection that represents depolarization of the atria. The PR interval is the time between the beginning of the P wave and the beginning of the QRS complex. The PR segment is the flat line between the end of the P wave and the start of the QRS complex. It represents time between atrial and ventricular activation. QRS complex is a distinct waveform that represents the rapid depolarization of the ventricles. The ST segment is a horizontal line that represents the interval between ventricular depolarization and repolarization. The T wave represents repolarization of the ventricles. The QT interval is the time from the start of the QRS complex to the end of the T wave, and represents the total time for ventricular depolarization and repolarization. The TP segment is the flat baseline that follows the T wave and precedes the next P wave. It represents the interval between ventricular repolarization and the next atrial depolarization.